A common theme among those suffering from certain mental health conditions is the tendency to isolate oneself. This can be driven by a number of factors but can also perpetuate the feeling of loneliness and fear, and result in an ongoing cycle of self-isolation. This was a topic that was recently discussed with a guest on the #FuturePsychiatryPodcast.
KEY TAKEAWAYS

- Mental illness can be a major contributing factor toward one’s tendency to isolate.
- As one isolates, mental illness may worsen, thus contributing to a self-perpetuating cycle.
What are some common reasons people with mental illness would isolate?

It’s clear that depression and anxiety change our perception of reality. One can be driven toward isolation for a number of reasons:
- Retirement
- Introversion trait; a chronic lack of desire to be around others
- Lack of energy to socialize
- Lack of opportunity to socialize
- Cognitive or sensory impairments that make it difficult to socialize
- Feeling disconnected or disassociated from others
- Feeling ashamed or anxious in front of others
- Feeling like a burden in social situations
- Feeling hypersensitive to rejection
Perhaps isolation can be conceptualized as one’s maladaptive way to focus all attention and energy on solving some inner problem. By isolating, it “feels” like you’re solving your problem by conserving all your energy and allowing yourself to spend every waking minute thinking about your issues. You perseverate. You ruminate. Your brain runs through thoughts on loop.
How difficult is being social while struggling with mental illness?
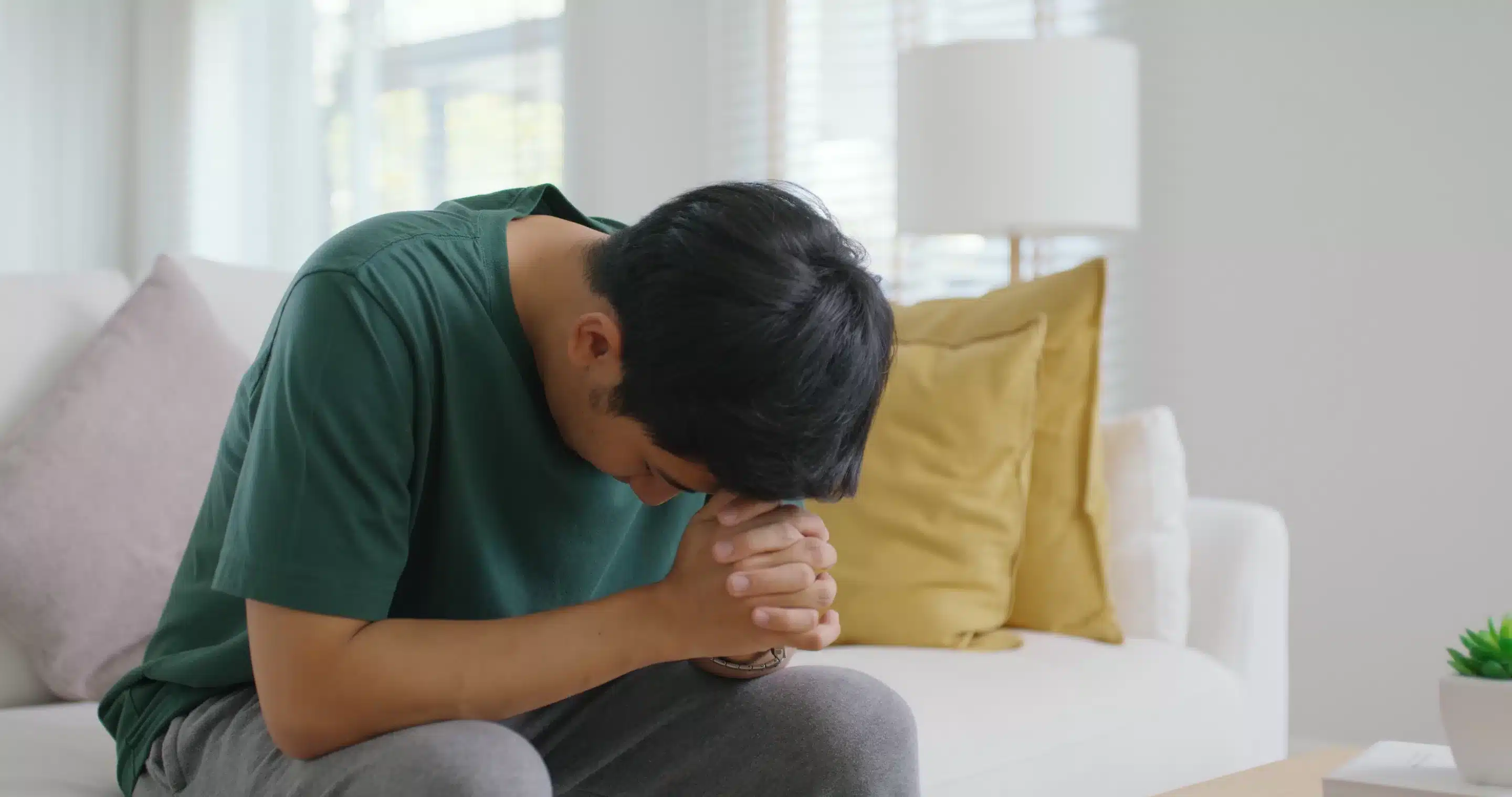
In addition, the stress involved and the energy it takes for someone to “perform” in front of other people is too much. The emotions we feel when we are dealing with mental illness are taxing and can exhaust us. Adding the pressures that come with being in social situations can feel overwhelming and so the default is to withdraw.
Isolating oneself is a coping mechanism, a way to protect oneself when we know that being around other people can be triggering to our condition. Being alone feels safer and more secure.
The Need to Have Some Control

Mental illness can be experienced as a loss of control of one’s feelings. When the chemicals in the brain are out of balance, certain hormones are released or repressed, and this has a direct effect over our perception of ourselves and the world around us. With no conscious input or means to prevent this, it can feel frightening to realize we are losing the ability to control these perceptions and the feelings that ensue.
Being withdrawn from society, from people, and from everyday activities is often the easiest way to regain a sense of being in control.
In one’s own company, with the door closed to the outside world, we limit the possibility for the familiar and unpleasant feelings to arise.
A Self-Perpetuating Vicious Cycle

Of course, the problem will often worsen with self-isolation. The more one isolates, the more one fears facing people.
Staying home and isolated feels safe and it can become less and less desirable to leave the comfort of one’s own room, or even bed. Exerting the energy involved in washing, grooming, and keeping one’s space clean and tidy can become more and more challenging.
Excerpt from the #FuturePsychiatryPodcast on isolation
The Importance of Breaking the Cycle of Isolation in Order to Heal

There is a fine balance between allowing a patient their much-needed space and leaving them to perpetuate their symptoms. Therefore, whether as a friend, clinician or support worker, it is vital to find ways of drawing the sufferer out of their safe zone, a little at a time.
To do this, it’s important to be mindful of the triggers that can send them back into isolation and work hard to counter these possible triggers.
Help them to feel worthy rather than worthless. Let them know that they can speak about their feelings and that these feelings matter. Encourage them out for limited periods, letting them know that there will be no pressure to stay out for longer than they are comfortable.
Broach the need for a little help to tidy their space or to get important admin done. And encourage them to make a little extra effort to look – and therefore feel – good.
No One Has to Feel Alone

It is important for sufferers of mental illness to stay connected with the outside world. Connection can help with recovery and prevent the condition from worsening.
Purposeful isolation in order to prioritize rest and self-care must be encouraged but reminding them that they aren’t alone and that there is a support network there for them is vital to help them along their journey to recovery.

If you are struggling with substance or alcohol use, depression, or anxiety, intensive outpatient may be right for you. Contact us at (888) 730-5220 or contact us to begin the process of healing today!









